Chronic Obstructive Pulmonary Disease (COPD) is more than just a breathing disorder; it’s a worldwide health challenge affecting over 390 million people and ranking as the fourth leading cause of death globally, with more than 3.5 million lives lost to COPD (WHO).


Beyond the alarming death toll, COPD places a massive economic burden on healthcare systems due to frequent hospitalizations, medications, and lost productivity. For patients, the impact is deeply personal because breathlessness, fatigue, and difficulty speaking can turn everyday tasks into exhausting challenges. These struggles often lead to reduced independence, frustration, and a lower quality of life.
That’s why researchers are now exploring new ways to help people with COPD breathe more easily and live better, including promising approaches such as RMT, which we’ll explore in this article through a peer-reviewed evidence-based study.
How does COPD affect your breathing, speech, and quality of life?
To understand why therapies like RMT are important, it’s essential first to examine how COPD affects the body and daily living.
Breathing: When every breath feels like work
COPD damages the airways, causing them to narrow, which makes it harder for air to flow in and out of the lungs. Over time, these narrowed airways, coupled with weakened breathing muscles, lead to chronic breathlessness (dyspnea) and reduced lung capacity. Imagine trying to breathe through a narrow straw; that’s what many COPD patients experience, especially during physical activity. As a result, many avoid exertion altogether, which can worsen muscle weakness and overall fitness.


Speech: The overlooked symptom
Speech might not be the first thing you think of with COPD, but it’s often affected. Speaking requires carefully coordinated breathing as you need enough airflow to sustain phrases and control volume. With COPD, patients often:
-
Speak more softly or with reduced volume
-
Take frequent pauses mid-sentence
Struggle to speak in long sentences without running out of breath [1]
This doesn’t just make communication frustrating, but it can also impact confidence, social interactions, emotional well-being, and voice-related quality of life in COPD patients. Some people with COPD avoid conversations altogether because it feels physically exhausting to talk.
Quality of life: More than just lungs
COPD’s effects ripple through every aspect of life. The limited mobility can lead to isolation, anxiety, and depression, as patients may feel embarrassed or fearful of breathlessness in public [2]. A systematic review of 10 studies found that nearly 55% of COPD patients report moderate-to-severe anxiety, with a higher percentage of women. [3]
Taken together, these physical and emotional burdens make COPD more than just a lung disease; instead, it’s a condition that reshapes a person’s entire lifestyle. This is why treatments that can improve breathing capacity and speech can help people feel more connected, active, and in control of their lives again.


Why Respiratory Muscle Training matters?
When we think about COPD treatment, most people picture inhalers, oxygen therapy, or medications. A few realize that their breathing muscles can be trained, just like their arms or legs.
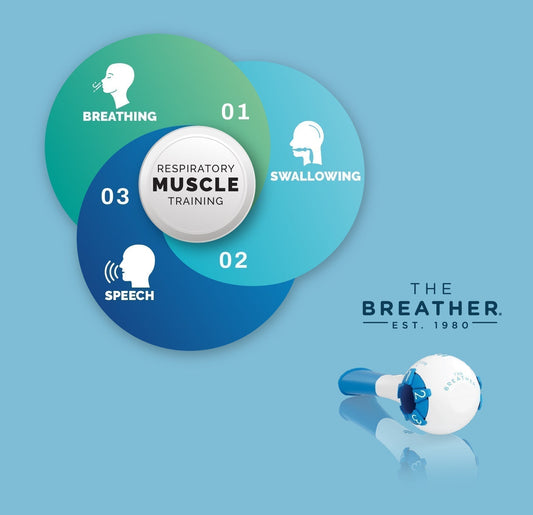
Respiratory muscle training is an isolation exercise for your breathing muscles, including the diaphragm (your primary breathing muscle) and the intercostals (muscles between your ribs). By using a simple handheld device that provides adjustable resistance, you “work out” these breathing muscles, gradually building strength and endurance.
Unlike traditional breathing exercises that focus mainly on technique or relaxation (such as pursed-lip breathing), RMT incorporates resistance into your breathing, resulting in the strengthening of your breathing muscles.
This is similar to lifting weights at the gym, which challenges the muscles and stimulates growth and adaptation. Over time, this can result in improved airflow, stronger coughs (essential for clearing mucus), and reduced effort required to take a deep breath.
The science behind RMT is compelling. A clinical study has demonstrated that with RMT, you can improve your breathing muscle strength and exercise tolerance in just two weeks of training.


Can RMT be done at home for COPD patients?
One of the biggest challenges in managing COPD is making treatments practical and accessible for patients in their everyday lives. Pulmonary rehabilitation programs are highly effective, but they require regular visits to a clinic that many patients struggle with due to mobility issues, transportation barriers, or scheduling conflicts. That’s why home-based RMT provides the best solution, offering a flexible, self-directed option that patients can integrate into their daily routine.
A recent study aimed to explore this very question. Researchers recruited patients with COPD receiving care in a home health setting and provided them with a structured RMT program. The participants used a clinically validated handheld device (THE BREATHER) to perform RMT with 2 sets of 10 breaths twice a day for a consecutive 28 days. [4]
Importantly, the home-based approach allowed patients to complete their sessions independently, with guidance and monitoring from the clinical team. This makes RMT highly feasible for people who may not be able to attend frequent hospital or rehab visits. The results, as we’ll see next, suggest that this home-based strategy can produce meaningful improvements that go beyond breathing alone.
What did the study find about RMT and COPD?
This study demonstrated statistically significant results, providing strong support for adding RMT to home-based COPD care. After completing the intervention, participants demonstrated measurable improvements in both lung function and speech performance—two areas that directly impact quality of life.


RMT improves lung function in COPD patients
The most striking results were the lung function tests. The COPD patients experienced a 92% improvement in peak expiratory pressure (from 190.7 L/min to 324.5 L/min) after 28 days of RMT, indicating a doubling of the strength of their expiratory muscles (the muscles used for breathing out). The stronger expiratory muscles facilitate the clearing of mucus and control airflow during speech.
RMT improves speech in COPD patients
At the same time, the COPD patients experienced a 116% increase in maximum phonation time (from 5.8 seconds to 12.1 seconds), indicating that patients were able to sustain phonation (the ability to produce sound) for more extended periods. The dramatic rise in MPT means patients could speak in longer, smoother phrases without running out of breath, a huge quality-of-life improvement for those who struggle to hold conversations.
How well did patients stick with the COPD program?
COPD patients didn’t just try RMT once and stop; they completed about 84% of all scheduled sessions over the four-week program. That’s a very high rate for any home-based health routine, especially for people managing a chronic condition. What’s even more encouraging is that many participants were able to gradually increase the resistance level on their devices. For patients wondering if they’ll be able to stick with RMT, this study shows that it’s not only doable but also rewarding enough to stay consistent.


Is RMT easy to do at home?
Yes — and that’s precisely what makes it so powerful for COPD patients. In this study, the entire program could be done at home in just a few minutes a day using THE BREATHER. No hospital visits, no special equipment, and no complicated setup, just two quick sets of 10 breaths, twice a day. Patients were able to follow the plan independently, demonstrating that RMT is not only effective but also practical for everyday life. For someone living with COPD, this means you can work on improving your breathing and speech from the comfort of your own home without disrupting your routine.
Why are these results important for COPD patients?
Numbers on any research paper don’t always capture what they mean for everyday life. However, in this case, the message is clear: improved breathing and longer speech times translate into greater freedom and confidence for patients with COPD. A 92% boost in peak expiratory pressure means your breathing muscles are stronger, so clearing your airways, climbing a flight of stairs, or even walking across the room can feel less exhausting. A 112% increase in maximum phonation time means you can talk for longer without gasping for air, making conversations smoother and less stressful.
Most importantly, RMT doesn’t replace medications or other COPD treatments; it complements them, adding another tool that empowers patients to take a more active role in managing their condition.
How can you get started with Respiratory Muscle Training?
Getting started with RMT is easier than most people think. The earlier you begin, the sooner you can see results. The first step is to consult with your doctor or respiratory therapist to determine if RMT is suitable for you. They can review your medical history to ensure it’s safe for your condition and even help you set initial resistance levels on your device.
Once you’re cleared to begin, choose a clinically validated device explicitly designed for COPD patients, such as THE BREATHER. This type of device enables you to train both inhalation and exhalation muscles, which is crucial for enhancing speech and overall lung function. Most effective RMT programs for COPD patients recommend a simple routine: two sets of 10 breaths, twice a day — a commitment of just a few minutes that can easily fit into your daily schedule.
For optimal results, be consistent and gradually increase the resistance as your muscles become stronger. If you ever feel dizzy, unusually fatigued, or short of breath, pause and check in with your healthcare provider. Safety is essential, especially for those with advanced COPD or other health conditions.
Quick start checklist
- Talk to your doctor or respiratory therapist.
- Get a clinically proven device like THE BREATHER.
- Follow a structured routine (10 breaths, 2 times a day).
- Increase resistance gradually as you get stronger.
- Monitor your progress and stay consistent.
By taking these steps, you’re not just starting a new exercise; you’re taking control of your breathing, your speech, and your quality of life.
What’s the bottom line on RMT for COPD?
COPD may be a lifelong condition, but it doesn’t have to control every part of your life. This study demonstrates that just a few minutes of Respiratory Muscle Training each day can strengthen your breathing muscles, enhance your ability to speak, and increase your confidence and independence. RMT is safe, practical, and easy to do at home, which makes it one of the most empowering tools available for people living with COPD.
If you’ve been looking for a natural, evidence-based way to support your breathing, now is the time to act. Discuss with your doctor the addition of RMT to your COPD management plan and explore tools like THE BREATHER to get started.
Frequently asked questions about RMT for COPD
Let’s see some of your common questions about RMT and COPD:
Can respiratory muscle training really improve COPD symptoms?
Yes! Multiple studies, including the one discussed in this article, showed that RMT strengthens breathing muscles, enhances airflow, and alleviates the sensation of breathlessness. It can also improve speech endurance, making it easier to maintain conversations without feeling breathless.
How long will it take me to see results with THE BREATHER in COPD?
Many patients notice improvements within just 4 to 6 weeks of consistent training with THE BREATHER. In the study, participants achieved a 92% increase in expiratory pressure and a 112% boost in speech duration after four weeks. Results may vary from individual to individual based on the severity of the disease, but consistency is key.
Is RMT really safe for severe COPD patients?
Generally, YES. RMT is considered safe for most COPD patients, even in moderate to severe stages, as long as it is done under medical guidance. Always consult your doctor before starting, especially if you have other conditions such as heart disease.
Can RMT replace inhalers or medications?
No. RMT is a complementary therapy, not a substitute for prescribed medications or inhalers. It works best as part of a comprehensive COPD management plan, which may include inhalers, pulmonary rehabilitation, and lifestyle modifications.
Can RMT reduce my need for medications or inhalers?
While RMT can improve breathing and reduce flare-ups, it should not be used as a replacement for your medications without your doctor’s approval. Over time, stronger breathing muscles may reduce symptoms and the need for rescue inhalers; however, treatment decisions should always be guided by your healthcare provider.
Can I do RMT at home without supervision?
Absolutely, YES. One of the biggest advantages of RMT is that it can be safely done at home. Most programs require only a few minutes per day and don’t need direct supervision, though your doctor may want to check in periodically to monitor your progress.
How often should I use THE BREATHER in COPD?
Most programs recommend two sessions per day, with each session consisting of two sets of 10 breaths. Over time, your resistance level can increase as your muscles become stronger. Consistency is the key to seeing lasting results.