We teach children to walk, talk, read, and ride a bike, but what about functional breathing? Breathing is the first thing we do when we’re born, yet if it becomes weak or uncoordinated, it can quietly hold a child back from thriving. The truth is, breathing isn’t just automatic; it’s a trainable act. And just like we strengthen arms or legs through therapy, we can strengthen the muscles that power every breath, word, and giggle. That’s the goal of Respiratory Muscle Training (RMT). Though often overlooked, RMT is becoming a powerful tool for children with asthma, developmental delays, speech challenges, or neurological conditions.
In this article, we’ll explore how RMT works in children, which conditions it can help with, how to get started safely, and why THE BREATHER is uniquely suited for pediatric use.


What is Respiratory Muscle Training in children?
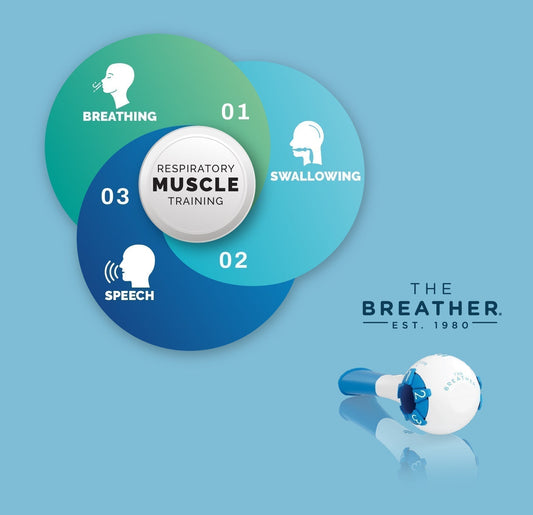
Breathing may feel automatic, but it relies on muscles that include the diaphragm, intercostals, and abdominals, all working in sync to move air in and out of the lungs. RMT strengthens these muscles by adding resistance to each breath, making them work harder and grow stronger over time.
Children typically don’t need to think about breathing, but in some instances, their breathing muscles may be too weak or poorly coordinated to support everyday activities. This can lead to shallow breathing, poor speech projection, limited stamina, and frequent respiratory infections. In these situations, RMT helps by turning each breath into a mini workout, offering a safe and structured way to improve the strength, endurance, and control of breathing muscles. When done consistently, it not only enhances respiratory function but also improves a child’s energy levels, posture, speech clarity, and even swallowing control.


These benefits aren’t just theoretical — they matter most when kids face health challenges. Let’s look at the conditions where RMT can be a game-changer
What are the conditions in which RMT can be beneficial for my kid?
As a parent, you know your child best. You notice when they struggle to catch their breath while playing, when their voice fades halfway through a sentence, or when mealtime becomes tiring instead of joyful. These everyday signs often point to something more profound: a need for stronger, more coordinated respiratory muscles. That’s where respiratory muscle training can help.
Below are everyday situations and conditions where parents often find RMT to be especially helpful for their child:
-
My child gets breathless easily during play or physical activity.
If your child avoids running, tires quickly, or frequently needs to pause and catch their breath, it could be due to poor respiratory endurance. RMT builds the breathing strength necessary for deeper, more efficient breathing, which can make activities easier for children and more enjoyable.
-
My child has asthma or reactive airway issues.
Children with breathing problems (asthma, COPD, and other chronic lung diseases) often develop shallow breathing patterns or weak exhalation muscles, especially after frequent flare-ups. RMT helps train the muscles used for both inhaling and exhaling, improving airflow, cough strength, and breath control during activities.
-
My child has trouble speaking clearly or loudly.
If your child runs out of breath mid-sentence, has a quiet or monotone voice, or struggles with articulation, RMT can help strengthen the muscles that support speech volume and clarity. It's commonly used alongside speech therapy for children with voice or articulation difficulties.


-
My child gags, chokes, or struggles while eating or drinking.
Breathing and swallowing are closely connected. RMT supports safer swallow patterns by building the muscles that help time breathing and protect the airway during meals, especially important in children with dysphagia or feeding challenges.
-
My child appears to be low-energy or sluggish most of the day.
Sometimes, poor oxygen exchange due to weak breathing muscles can lead to low energy, impaired concentration, or even disrupted sleep. RMT helps improve breathing efficiency, which may support better focus, stamina, and restfulness.
-
My child has low muscle tone or developmental delays.
Some conditions, like Down syndrome, bronchopulmonary dysplasia, hypotonia, or motor delays, can affect core and breathing muscles. RMT helps build tone, stability, and respiratory coordination, supporting posture, endurance, and even transitions between sitting and standing.
-
My child was born prematurely or has underdeveloped lungs.
Premature birth may leave a child with weaker lungs and less mature respiratory muscles, even when they grow up. If your child still struggles with feeding, fatigue, or breathing during exertion, RMT may help them catch up, improving breath depth, oxygenation, and muscle coordination.


-
Are there any medical or genetic conditions in which RMT can help my child?
Sometimes the need for RMT isn’t just about everyday challenges, but is also linked to diagnosed medical conditions. Here’s when RMT becomes especially helpful. Children diagnosed with conditions such as Cerebral Palsy, Down Syndrome, Muscular Dystrophy, Premature birth complications, Spinal cord injuries, Developmental delays, or obesity may benefit from RMT. These conditions frequently involve low muscle tone, poor coordination, or inefficient breathing, all of which RMT is designed to improve.
(Safety Reminder: Never start RMT on your own if you have these conditions. Always work with a healthcare professional to ensure it is safe and effective for you.)
9. What is the minimum age for kids to start RMT?
Most children can begin RMT as early as 5 years old, as long as they can follow simple instructions such as “breathe in,” “breathe out,” or “blow steadily.” (PMID: 39229292) At this age, kids can understand basic cues and participate in short, playful training sessions without frustration. As long as the child can cooperate, maintain a seal on the mouthpiece, and engage safely, RMT can be introduced gradually and effectively.


Parents often ask: Does RMT really work? Fortunately, science has many answers. Researchers have studied RMT in children with many of these conditions, and the results are promising.
How RMT works for kids: The science explained.
Children are often full of energy, but when their breathing muscles are weak, even simple tasks can feel tiring, including climbing stairs, speaking a sentence, or chewing food. That’s because breathing isn’t just about the lungs; it’s powered by a system of muscles that need strength, coordination, and endurance.
RMT works by applying resistance to either inhalation, exhalation, or both - essentially making the respiratory muscles work harder with every breath. Over time, this repeated resistance strengthens the diaphragm, intercostal muscles, and other accessory muscles that are responsible for drawing air in and supporting forceful exhalation.
Best of all, RMT is designed to meet children where they are. The intensity can be adjusted based on age, diagnosis, and developmental level, ensuring that each child receives a safe and progressive challenge that supports their abilities.
Hearing about research is reassuring, but you may still wonder — is it safe for my child to do this at home? Here’s what experts and studies say about RMT safety.
Is RMT safe and effective for children?
Whenever we introduce a new therapy into a child’s care plan, two questions arise first: “Is it safe?” and “Does it really work?” When it comes to RMT, the answer to both is a confident "YES".
RMT has been studied across a range of pediatric populations, from children with neuromuscular disorders to those with asthma, cystic fibrosis, and developmental delays. Clinical research indicates that RMT can even improve respiratory muscle strength, peak expiratory flow (essential for coughing and airway clearance), and overall breathing efficiency in young children. [1] For children with chronic conditions, this often translates into improved endurance, reduced respiratory infections, and enhanced participation in daily activities.
One of the key reasons RMT is considered safe is its adaptability. Even more reassuring is how well children tend to respond. Unlike many therapies that feel like hard work, RMT is often seen as a challenge or even a game, especially when progress becomes visible.
Improvements in speech volume, stamina, and breathing ease can be felt within weeks, reinforcing motivation and cooperation. It’s a rare kind of therapy that blends measurable progress with a sense of empowerment.
These real-world outcomes, supported by both data and clinical experience, have led many pediatric therapists and physicians to include RMT as a core part of respiratory rehabilitation. And as we’ll see next, there are case studies that bring these benefits to life in ways the data alone can’t capture.
Beyond general safety, researchers have explored RMT in depth — across different diagnoses, ages, and therapy settings. Here’s what the data tells us.
What is the scientific evidence for RMT in children?
Over the past two decades, Respiratory Muscle Training (RMT) has been evaluated in children with a wide range of health conditions, and the results are consistently encouraging. Research has shown that RMT can benefit:
Active healthy children may also benefit from RMT by increasing their aerobic fitness (PMID: 36429439), as they are more prone to respiratory fatigue. RMT has been shown to improve lung and breathing function in young swimmers (PMID: 15942767), swimming performance in events shorter than 400m (PMID: 19841931), and breathing muscle strength in well-trained youth swimmers (PMID: 31344014). A 2013 study showed that RMT can improve ventilatory function parameters, chest expansion, respiratory muscle strength and endurance, performance, exertion, and dyspnea in young, well-trained swimmers (PMID: 24421721). In addition to swimmers, RMT has also proven to improve breathing muscle strength and aerobic endurance in young soccer players in a 2019 study (PMID: 31905644), as well as breathing muscle strength and endurance, exercise tolerance, and aerobic fitness in amateur indoor soccer players (PMID: 33307554).
Children with neuromuscular disease have weak breathing muscles that can put them at risk of morbidity and mortality. RMT helps strengthen weak breathing muscles. Let's look at the scientific evidence for that. A 2017 systematic review (PMID: 28462787) including children and adolescents with neuromuscular diseases found that RMT significantly improved breathing muscle strength and endurance. Another 2019 systematic review (PMID: 31487757) of 11 clinical studies with 250 individuals with neuromuscular diseases showed that RMT may improve lung capacity and respiratory muscle strength. Going forward, a 2024 clinical trial (PMID: 39229292) in children with neuromuscular disorders showed that performing RMT for 3 months significantly improved breathing muscle strength and cough effectiveness.


Asthma often causes breathing muscle weakness and inefficient breathing patterns, which can worsen symptoms. Asthma-related airway inflammation and bronchoconstriction increase the work of breathing, putting extra strain on the breathing muscles, especially the diaphragm. RMT helps strengthen the breathing muscles, making breathing easier and more efficient. A 2024 meta-analysis (PMID: 38562138) combined results from six different trials involving 333 kids and looked at how RMT helps children with asthma breathe better. The main finding was that RMT strengthened the breathing muscles and improved lung function in children with asthma.
Children with cerebral palsy often have weakness, stiffness, or poor coordination of the breathing muscles, resulting in poor breaths, reduced lung capacity, reduced cough strength, along with swallow and speech issues. However, a recent 2024 meta-analysis (PMID: 38568267) reported that RMT improved breathing muscles in children with cerebral palsy.
Children with Down Syndrome often face low muscle tone (hypotonia) and unique airway anatomy that affects breathing, leading to weak breathing muscles, a high risk of airway collapse, frequent respiratory infections, and low exercise tolerance. A 2022 clinical study (PMID: 35533737) demonstrated that children with Down Syndrome who underwent RMT and aerobic exercise showed significant improvements in breathing muscle strength, aerobic endurance, and overall muscle strength compared to those who performed aerobic exercise alone.
Obesity in children and adolescents is associated with decreased respiratory muscle strength and reduced lung capacity, resulting in increased shortness of breath during physical activity. In obese adolescents, adding respiratory muscle endurance training to a standard weight-loss program reduced the oxygen cost of cycling and the perceived exertion during higher-intensity exercise compared to weight loss alone (PMID: 28747408). Another 2018 randomized control study (PMID: 30350405) showed that a short-term (3-week) respiratory muscle endurance training program significantly reduced the oxygen cost of walking and improved exercise tolerance in obese adolescents. An eight-week RMT improved both inspiratory muscle strength (MIP) and functional fitness (6-MWT) in children/adolescents with obesity (PMID: 35874588).


Cystic fibrosis is a genetic disorder characterised by the production of thick, sticky mucus that primarily affects the lungs, pancreas, and other organs. This thick mucus clogs the airways, leading to chronic lung infections and inflammation that can cause difficult breathing. RMT in children and adolescents with cystic fibrosis significantly improves inspiratory muscle strength (PMID: 38622583) that may enhance breathlessness, exercise tolerance, support more effective airway clearance, and delay respiratory fatigue, ultimately improving overall quality of life and daily functioning.
Together, these findings confirm that RMT is not just a theoretical tool—it has a real, measurable impact across different pediatric groups. While the goals may vary, the underlying principle is the same.
With so much evidence supporting RMT, the next step is knowing how to do it correctly. Here’s what research and therapists recommend for children
What is the correct protocol of RMT for my child?
Children and young people should train at a slightly lower intensity than adults. The target RMT intensity is 30% to 50% of MIP/MEP (Maximum Inspiratory Pressure/Maximum Expiratory Pressure), although higher intensities may be suitable for particular groups (PMID: 36033343).


Training protocols need to be adjusted according to the disease. RMT sessions of 10 to 20 minutes, with rest periods of 1 to 3 minutes every 5 to 6 days per week, have proven effective. RMT should be maintained for at least 4 weeks. RMT should always be supervised if your child has a condition or disease.
What are the tips for parents and pediatric therapists starting RMT?
Starting RMT with children can feel like stepping into uncharted territory, but with the right approach, it becomes a powerful and rewarding part of care. This section will guide you through essential strategies to help parents and pediatric therapists confidently implement RMT at home or in clinic settings.


If you’re thinking, 'This sounds great — but how do I get started?'
Choosing the right RMT device for Kids
Not all RMT devices are created with children in mind. The ideal device for children's use should offer low initial resistance, adjustable settings, and be easy to use and handle. Devices that are durable, easy to clean, and visually simple also tend to be more acceptable for both children and their parents.
Most importantly, the choice should be made in collaboration with the care team, ideally a speech-language pathologist, occupational therapist, or respiratory therapist familiar with pediatric needs.
Making RMT fun and engaging for children
The success of any therapy for kids is hidden in the fact that it shouldn’t feel like a chore. Children are more likely to stick with RMT when it’s disguised as a game or play. Try turning sessions into mini-challenges: who can blow the longest, or make the loudest “dragon roar”.


Visual aids, such as progress charts, sticker rewards, or interactive breathing games using simple props, can help maintain high motivation. Music, silly sounds, and sibling involvement can also make sessions feel less clinical and more like a fun family activity.
How to track the progress of RMT over time for children
Tracking outcomes is essential not just for clinical feedback but for encouraging children and caregivers alike. Objective measures, such as Peak Cough Flow, Maximal Inspiratory Pressure, or simply counting how long the child can sustain a breath or blow, can offer visible signs of progress.
At home, parents can use basic trackers: weekly logs, simple rating scales (“How easy was breathing today?”), or even drawing smiley faces based on effort and fun. Therapists may use more formal tools, such as spirometry, video analysis, or voice quality assessments, depending on the specific goals of the treatment.
Why choose THE BREATHER for RMT in KIDS?
When it comes to RMT for children, the tool you choose can make all the difference. That’s where THE BREATHER stands out, not just as a device, but as a thoughtfully designed companion in a child’s journey toward better breathing. Let’s explore what makes it the go-to choice for pediatric RMT.


Features that support pediatric use of THE BREATHER
Children aren’t just small adults; they need tools that are tailored to their size, behavior, and comfort. THE BREATHER has the following characteristics that make it loved by children:
-
It is lightweight and compact, making it easy for little hands to hold and use.
-
Its adjustable resistance dials offer precise control, allowing therapists or parents to start at the lowest setting and progress gradually as the child improves.
-
It is non-electronic and free of screens or batteries, which reduces distractions and makes it safe and intuitive for younger users.
-
The soft silicone mouthpiece is comfortable for small mouths, and its durable, medical-grade materials can withstand the drops and tugs of daily pediatric use.
What sets THE BREATHER apart?
While there are other RMT devices on the market, very few cater to the unique needs of children. THE BREATHER stands apart due to its dual-function design, which trains both inspiratory and expiratory muscles in one device. This is especially valuable for kids dealing with complex respiratory issues, as it offers a more holistic approach to strengthening their breathing.
Breathing may seem simple, but when it works better, kids thrive. Here’s what to remember as you consider RMT for your child.
Final thoughts
Breathing is life’s most essential skill, and like any skill, it can be strengthened. RMT offers a science-backed, kid-friendly approach to help children breathe more easily, play harder, speak more clearly, and recover faster. Whether your child has asthma, developmental delays, or struggles with endurance, RMT is a safe, proven approach that meets them where they are.
With the proper guidance and tools, like THE BREATHER, you can turn every breath into a step toward better health, confidence, and independence. If you’re ready to explore RMT for your child, speak with your pediatric therapist or healthcare provider about starting a simple, personalized program today.
References
[1]. Inspiratory Muscle Rehabilitation Training in Pediatrics: What Is the Evidence?