Breathing, speaking, and swallowing might seem like separate tasks, but they are more closely connected than most people realise. These vital functions share overlapping anatomy and must be precisely coordinated to prevent issues like aspiration, voice disorders, or pneumonia. [1] Understanding how they interact is essential, especially when you have to address conditions like dysphagia or speech problems.
In this article, you’ll explore this critical connection between these three functions and how RMT can support better function and quality of life.
To begin understanding the connection between these systems, let’s first look at how breathing and swallowing must work together to keep the airway safe.


Breathing and swallowing coordination: Protecting your airways
The swallowing reflex is actually a complex, multi-step, patterned response that involves voluntary and involuntary actions. It is an innate (inborn) reflex, while learning and experience do play a role in refining and coordinating the voluntary aspects of swallowing.
As breathing and swallowing share the same anatomical pathway (mouth and throat), these two functions must be precisely timed to maintain ventilation during food intake and to prevent aspiration. Aspiration occurs when food or liquid accidentally enters the airways instead of passing into the esophagus. Prevention of aspiration is highly dependent on a correct breathe-swallow pattern. [2]


Now that we understand the importance of this coordination, let’s examine the swallowing process in more detail and explore why each phase plays a crucial role.
What are the stages of swallowing
Swallowing can be divided into several phases.
Anticipatory phase: You visually analyse the food and your brain creates a plan for swallowing based on the texture, taste, and consistency.
Oral phase: Your mouth analyzes the food, confirming the visual expectation, purees it, and moves it backward into your throat.
Pharyngeal phase: You move the food into the esophagus, bypassing the airway.
And when that rhythm is off, even slightly, the risk of aspiration and other complications rises, especially in people with weakened respiratory or neurological function.
Now that you see how finely tuned the swallowing process is, it’s easier to understand why even minor disruptions can have significant consequences.
Why do people with swallowing problems (dysphagia) aspirate more often?
If any phase of swallowing or its coordination is disrupted, the risk of aspiration increases. If you are a healthy individual, aspiration triggers the cough reflex, and the food is expelled. However, if you have swallowing dysfunction, aspiration occurs frequently, often in combination with impaired cough function.
This inefficient airway hygiene can lead to the development of pneumonia, as food debris in the lungs provides a breeding ground for bacteria, as well as to malnutrition, as patients learn to avoid foods that can lead to aspiration.
Swallow dysfunction is common in people with neurological or neuromuscular conditions such as Parkinson’s disease, multiple sclerosis, and stroke. Moreover, it is also seen in healthy older adults.


So, if the natural pattern breaks down, is there a way to restore it? The answer lies in how we retrain both breath and muscle memory.
What is the ideal breathe-swallow sequence?
In most healthy individuals, breathing and swallowing follow a precise and protective pattern. [3]
-
Brief inhale: Taking a short breath in before swallowing helps prepare the system.
-
Exhale slightly: Most swallows are initiated during the exhalation phase of breathing.
-
Swallow without breath (swallowing apnea): Breathing stops for about 0.5 to 1.5 seconds. The vocal cords close, and the larynx elevates to close the airway. The epiglottis folds over the airway to protect it.
-
Resume exhalation: After swallowing, a small exhalation follows, which helps clear any residue from the airway entrance.
However, in people with dysphagia (swallowing dysfunction), this pattern often becomes disrupted. Swallowing may occur during inhalation or at inappropriate lung volumes, increasing the likelihood that food or liquids will be misdirected into the airway.
In these cases, reestablishing the correct sequence is a crucial therapeutic goal. Rebuilding the pattern starts with retraining the sequence itself, and one foundational technique is helping patients do just that, one breath at a time. Let’s learn how to do that properly.
How do therapists teach the inhale–exhale–swallow technique?
Speech-language pathologists and therapists work with patients with swallowing dysfunction to retrain the swallow-breathe pattern through a structured, intentional approach that includes:
-
Inhale gently
-
Exhale slightly
-
Swallow during early exhalation, at the optimal lung volume
By consciously practicing this sequence, patients gradually rebuild the automatic coordination between breathing and swallowing. Restoring this coordination reduces the risk of aspiration and enhances overall meal safety. [4]
But timing isn’t the only issue; without the breathing strength to protect the airway and generate an effective cough, even perfect coordination falls short.
Why does the strength of breathing muscles matter for swallowing safety?
Correcting the swallow-breathe pattern isn’t just about timing; it’s also about physical capability. Patients with weakened breathing muscles or impaired cough function often struggle to protect their airways, even when the timing is correct. That’s why breathing muscle strengthening is a vital part of dysphagia therapy.
Enhancing respiratory strength benefits swallowing in several ways, as it:
-
Improves activation of muscles in the neck (suprahyoid muscles) that effectively move the hyoid bone and larynx, which protects the airway during swallowing [5][6]
-
Increases ribcage flexibility by strengthening the muscles involved in expanding the rib cage, which supports better inhalation volume before the swallow [7]
-
Boosts cough strength to facilitate the effective expulsion of aspirated material, if necessary. [8][9][10][11][12]
-
Supports airway clearance and pulmonary hygiene, reducing infection risk [13]
Without adequate respiratory support, even minor swallowing difficulties can escalate into serious health concerns like pneumonia, malnutrition, and dehydration.
That’s where respiratory muscle training comes in, not just as a strength builder, but as a tool to reinforce safe swallowing patterns long term.


How does respiratory muscle training support swallowing rehabilitation, according to the scientific evidence?
One highly effective method for strengthening the respiratory system is RMT, a form of resistance exercise for the breathing muscles.
Benefits of RMT for swallowing include:
-
Enhanced airway protection through stronger laryngeal function [5]
-
Improves cough strength and reduces the risk of aspiration [8][9][10][11][12][14]
-
Improved lung volumes to support optimal swallow timing [7]
The beneficial effects of RMT for individuals with dysphagia are supported by science and research. A 2025 clinical trial demonstrated that stroke patients who underwent RMT, in conjunction with other treatments, showed improvements in swallowing and experienced fewer aspiration problems [14].
Another 2025 meta-analysis including 10 clinical studies showed that RMT improved respiratory and swallowing function in elderly patients with dysphagia and reduced the risk of aspiration [15].
Similarly, a 2024 clinical trial involving 28 healthy adults demonstrated that RMT enhanced the strength and mass of the swallowing muscles, as well as the strength of breathing muscles [16].
Additionally, another 2020 study found that a 4-week combined respiratory muscle training (cRMT) using THE BREATHER significantly improved swallow function and airway protection in stroke patients with dysphagia [17].
Additionally, the RMT devices like THE BREATHER provide targeted training for both inspiratory and expiratory muscles, making them ideal tools in swallow rehabilitation. With consistent use, it can help patients recover a safer, more effective swallowing function, while reducing their risk of aspiration, malnutrition, and respiratory infections.
Interestingly, the same system that powers safe swallowing also fuels another essential function: the ability to speak clearly and confidently.
Breathing and Speech: How the lungs shape your voice
Just as swallowing relies heavily on a finely tuned respiratory system, speaking does as well. The process of phonation (the generation of sound) requires precise coordination between the larynx (voice box) and the upper and lower airways.
The chest wall (which includes the rib cage, sternum, thoracic vertebrae, diaphragm, and intercostal muscles) is especially vital during speech. Unlike quiet breathing, which is passive and rhythmic, speech breathing is an active process that must maintain consistent muscular pressure to sustain subglottic pressure (the air pressure beneath the vocal cords).
This pressure is crucial for maintaining the vibration of the vocal folds and producing clear, audible speech. The effectiveness of the chest wall during speech depends on the volume of the lungs. At high lung volume, maintaining high pressure is easier than at low lung volume, where the expiratory muscles must work harder to achieve the same effect. [18]
Just as we saw with swallowing, lung volume forms the foundation, and for speech, it can mean the difference between projection and strain.
Why do people with low lung volume struggle with speech?
Speech is usually initiated at higher lung volumes, about twice that of a resting breath. At these elevated volumes, it's easier for the respiratory muscles to generate the necessary pressure to support speech. As lung volume decreases, the effort required to maintain pressure increases, resulting in a weaker and more strained voice. [19]
Initiating speech at a low lung volume can lead to reduced vocal intensity, voice fatigue, short phrases with frequent breath interruptions, and a perception of vocal effort or discomfort. [20]


This pattern can be particularly noticeable in individuals with dysphonia (voice disorders), which affects 12% of adults [21] and 18% older adults [22] in the USA. Dysphonia not only affects vocal quality but can also cause emotional distress, social withdrawal, and diminished job performance, especially in professions that require sustained vocal output (e.g., teachers, call centre agents, singers, performers).
While lung volume drives vocal strength, the diaphragm quietly orchestrates the pressure shifts that make connected speech smooth and expressive.
What role does the diaphragm play in voice control?
The diaphragm also plays a crucial role, serving as the primary muscle for breathing support. It adjusts the pressure during changes in lung volume and promotes rapid inspirations during connected speech. [18] Activation of both inspiratory and expiratory muscles together provides the best control of chest wall function and optimal speech support.


However, when this coordination falters, whether due to weakness, tension, or misdiagnosis, the overlap between breath and voice can become a source of inconvenience.
Breathing and Voice Disorders: When Systems Misalign
Coordination between the respiratory system and the larynx is a delicate process. When disrupted, it can contribute to or worsen both voice disorders and respiratory conditions. There’s often a comorbidity between laryngeal and pulmonary dysfunctions.
For example:
-
Asthma and muscle tension dysphonia (MTD) mostly overlap and can mutually contribute to disease burden. A study showed that 66% of asthmatic patients showed MTD [23], while another study reported that 51% of the asthma patients showed MTD symptoms [24]. Additionally, another study reported that about 87% of patients with severe asthma had laryngeal dysfunction [25].
-
Disorders such as paradoxical vocal fold movement disorder (PVFMD) mimic symptoms of asthma or COPD, including shortness of breath, wheezing, or chest tightness. [26] Misdiagnosis is common because the symptoms overlap.
-
Individuals with respiratory muscle weakness often struggle to sustain phonation, which can lead to voice fatigue and reduced vocal stamina.


While the exact causal relationship between respiratory and voice disorders isn’t always clear, the overlap in symptoms and anatomical mechanisms makes it critical to evaluate and treat them together.
Just as with swallowing, respiratory muscle training provides valuable support for individuals seeking to restore vocal strength and clarity.
How respiratory muscle training supports speech therapy
A growing body of evidence supports the use of respiratory muscle training to complement speech therapy, especially in cases where poor breath support is a contributing factor. [27]
By using devices like THE BREATHER, individuals can strengthen their breathing muscles that can complement speech therapy. In a 2023 study published in the “Journal of Voice”, participants with voice disorders (dysphonia) who performed respiratory muscle training with THE BREATHER for 28 days showed improvements in voice and lung functions compared to those not using the device [28].
Speech therapists often recommend RMT as part of an integrated treatment plan for voice rehabilitation. Just a few minutes of consistent training per day can yield noticeable improvements in speech capacity and quality, particularly in older adults or individuals recovering from respiratory illness.
![]()
![]()
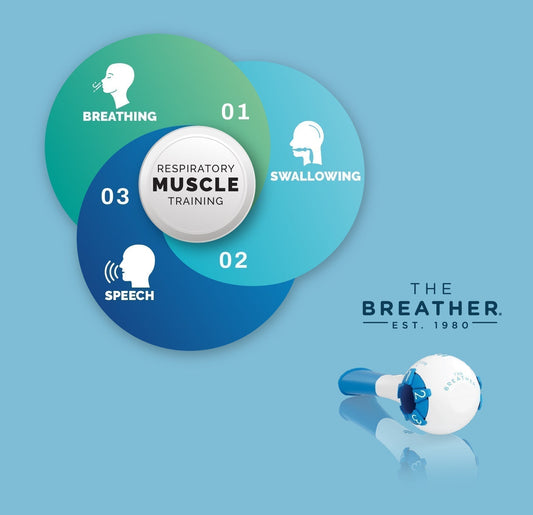
Across each of these functions, breathing, swallowing, and speaking, the same muscles, patterns, and pressures play a role. And when appropriately supported, they unlock better health and communication.
Conclusion: One breath powers many functions
Breathing, swallowing, and speech are not isolated actions but intricately connected functions that rely on precise muscular coordination due to shared anatomical pathways.
Disruptions in this coordination, whether due to aging, neurological conditions, or respiratory disorders, can lead to severe consequences, including aspiration, pneumonia, or voice problems.
Fortunately, targeted therapies like RMT can help strengthen the respiratory system, restore proper timing between breathing and swallowing, support safe airway protection, and improve vocal quality. By understanding how these systems work together and supporting them through intentional training, individuals can reclaim essential functions that are critical to health, communication, and quality of life.
Frequently Asked Questions (FAQs)
Here are some quick answers to help you understand how breath, speech, and swallow work together.
What is speech breathing, and why is it different from regular breathing?
Speech breathing involves controlled exhalation and increased lung volume to support vocalization, unlike quiet breathing, which is a passive and rhythmic process.
Can poor breathing affect my voice?
Yes, insufficient breath support can lead to a weak, strained, or breathy voice. It also increases vocal fatigue and reduces the length of phrases during speech.
How does THE BREATHER help with speech?
It helps strengthen the respiratory muscles needed for effective speech breathing. This improves breath control, projection, and vocal clarity.
Are voice and respiratory disorders connected?
Often, yes. Many people with voice disorders also have respiratory issues like asthma or airway restriction, and vice versa. A holistic approach is essential for treatment.