Obesity is a prevalent health concern with far-reaching implications for both individuals and society at large. In the United States, nearly half of all adults aged 20 or above are classified as obese, and this epidemic shows no signs of abating.
In this blog post, we’ll delve into the staggering statistics surrounding obesity and its profound impact on health and the economy.
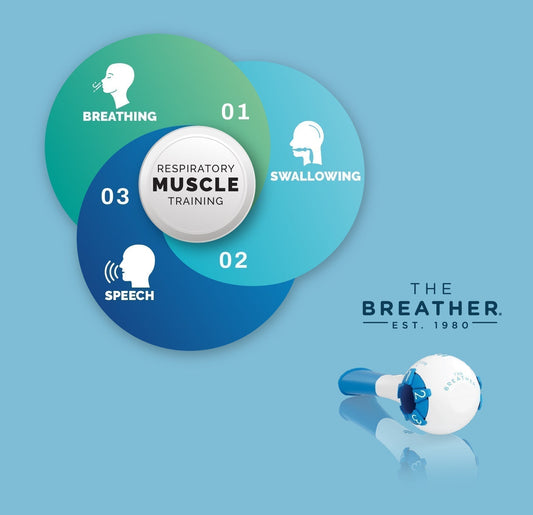
Additionally, we’ll explore the intriguing connection between cardiorespiratory fitness (CRF) and obesity, shedding light on how respiratory muscle training (RMT) could be a game-changer in the fight against excess weight.
The alarming statistics of obesity
Let’s begin with a sobering fact: about 43% of adults in the United States are currently grappling with obesity, while an additional 31% fall into the overweight category. Within this cohort, 9% face the harsh reality of severe obesity. Unsurprisingly, these figures have grave implications for health, well-being, and healthcare expenditure [1].


The geographical distribution of obesity in the U.S. reveals some striking disparities. West Virginia leads the pack with a staggering 40% of its population classified as obese, while Massachusetts boasts the lowest obesity prevalence, with just 28% [2].
What is the economic toll of obesity?
Obesity doesn’t just affect individuals—it also places an enormous economic burden on society. The annual medical costs associated with obesity amount to a staggering $172.74 billion [3].
Beyond direct medical expenses, the indirect costs due to decreased economic productivity are equally concerning. In 2016, obesity and its associated chronic diseases incurred $480.7 billion in direct healthcare costs and a jaw-dropping $1.24 trillion in indirect costs. This total of $1.72 trillion represents a staggering 9.3% of the United States’ gross domestic product [4].
What is the relationship between CRF and obesity?
Cardiorespiratory fitness (CRF) emerges as a crucial indicator of obesity. Obesity can lead to reduced lung and chest wall compliance, resulting in decreased functional residual capacity and expiratory preserved volume [5] [6].
This means that individuals with obesity typically breathe with reduced lung volume compared to their healthier counterparts. Consequently, they often exhibit lower CRF and energy expenditure, which can manifest as early fatigue, exertional dyspnea, and increased oxygen cost during exercise [7] [8] [9].
Exploring treatment options for losing weight
Addressing obesity necessitates a multi-faceted approach, including both pharmacological and non-pharmacological interventions [10].
Anti-obesity drugs, while effective in curbing appetite, can raise concerns about potential cardiovascular or psychiatric side effects with long-term use [11].
Non-pharmacological strategies include bariatric surgery, dietary modifications, cognitive behavioral interventions, and exercise [12].


What is the role of respiratory muscle training in weight loss?
Respiratory muscle training offers a novel approach to assist individuals suffering from obesity on their weight reduction journey or in improving daily mobility [13]. A recent clinical study showed that RMT helps weight reduction in individuals with obesity who trained with THE BREATHER for 2 weeks.
RMT strengthens respiratory muscles, reducing breathlessness—a common obstacle for individuals struggling with obesity during exercise. This reduced breathlessness can enhance exercise tolerance, a crucial component of successful weight loss [14].
Furthermore, RMT can benefit those with limited mobility, making daily activities more manageable and improving overall mobility and exercise tolerance [15].
Crucially, RMT can contribute to improved CRF, facilitating better performance during weight loss exercises. It’s important to note that RMT isn’t a standalone strategy for significant weight loss but rather an adjunct therapy that complements comprehensive weight loss programs involving nutritional control and exercise [16].
Conclusions
The obesity epidemic presents a substantial challenge to both individual health and the broader economy. Cardiorespiratory fitness plays a pivotal role in understanding and addressing this issue, with respiratory muscle training offering a promising avenue for improvement.
By addressing breathlessness and enhancing CRF, RMT can make a meaningful contribution to the fight against obesity.
References
[5]. Lin CK, Lin CC. Work of breathing and respiratory drive in obesity. Respirology. 2012;17(3):402–11.