Respiratory muscle training (RMT) has emerged as a non-invasive, drug-free solution for improving breathing strength and lung function in healthy individuals, athletes, or people with pulmonary or other diseases. Among the RMT devices available today, two technologies dominate:
-
Flow-based resistive RMT devices (like THE BREATHER)
-
Threshold RMT devices
Both have their places in breathing therapy, but which one delivers better clinical outcomes, enhances quality of life, and supports a more natural, sustained breathing pattern?
Let us compare and break it down.


Resistive vs. Threshold RMT Devices: What’s the Difference?
Before we go into the details of clinical evidence for these two devices, let's see how their function differs.
Threshold RMT devices
These devices use a spring-loaded valve that remains closed until you generate enough pressure to open it. Once the pressure is surpassed, the airflow becomes unrestricted, and you can complete the remaining breath with minimal resistance.
The threshold pressure is usually achieved within the initial 20% of the inspiratory volume, which results in a specific breathing pattern with a sharp and brief pressure peak followed by a neutral breathing phase with low effort.
Flow-based resistive RMT devices
These devices do not use a spring valve but an adjustable orifice to create dynamic resistance throughout inhalation. This means the muscular engagement remains consistent throughout the inhalation, utilizing the entire inspiratory volume for muscle training. THE BREATHER applies the same principle to the expiratory flow, targeting both inspiratory and expiratory muscles.
Scientific Comparison: Clinical trials speak volumes
Four independent research studies, conducted at different locations and times, directly compared the efficacy of resistive RMT devices and threshold RMT devices in a total of 198 COPD (Chronic Obstructive Pulmonary Disease) patients. The table below offers a summary overview, while the detailed explanations of each study follow.
Comparison of Key Studies: Resistive vs Threshold RMT Devices
| Studies | Patients | Training | Common benefits of both Devices | Benefits of the Resistive RMT Device only |
|---|---|---|---|---|
| The 2003 study (PMID: 12833187) | 30 | Two 15-minute sessions, 5 d/w for 8 weeks | Improved breathing muscle stamina and exercise capacity | Cost-effectiveness |
| The 2007 study (PMID: 17692243) | 33 | Two 15-minute sessions, for 6 weeks | Improved breathing muscle functions and health-related quality of life | Improved health-related quality of life |
| The 2017 study (PMID: 29229110) | 60 | Two 15-minute sessions, for 8 weeks | Improved breathing muscle strength, breathlessness, maximal exercise capacity, and quality of life | Improved quality of life and exercise capacity |
| The 2024 study (PMID: 39089392) | 75 | Two 15-minute sessions, for 8 weeks | Improved exercise capacity, breathing muscle strength, and breathlessness | Improved breathlessness, promoted deeper and slower breathing |
The 2003 study:
A study published in the “Journal of the Formosan Medical Association” compared the resistive RMT devices and threshold devices for the first time. Thirty patients with moderate to severe COPD were divided into three groups:
-
The first group used a resistive RMT device
-
The second group used a threshold RMT device
-
The third group didn’t perform RMT
The patients performed 15 minutes of RMT, twice a day, 5 times a week, for 8 weeks.
After the study period was completed, breathing muscle stamina (respiratory muscle endurance time) and exercise capacity (6-minute walking distance) were significantly improved in both the resistive RMT group and threshold RMT group compared to the control group.
Additionally, there was no difference in the efficacy of resistive RMT and threshold RMT devices, which clearly indicates that both devices equally benefited COPD patients. However, the patients appreciated the cost-effectiveness of the resistive RMT device [1]
The 2007 study
After four years, another study compared the effect of resistive RMT and threshold RMT in COPD patients performing two 15-minute training sessions daily for 6 weeks. In this study, thirty-three moderate to severe COPD patients were divided into three groups:
-
The first group performed resistive RMT
-
The second group performed threshold RMT
-
The third group performed SHAM training (using a similar breathing device but without the intended effect)
Both the resistive RMT group and the threshold RMT group showed significant improvement in breathing muscle functions and health-related quality of life in COPD patients.
Among the two training groups, the patients using the resistive RMT device reported significant improvements in all four aspects of health-related quality of life, including breathing difficulty, fatigue, emotions, and confidence in managing symptoms (mastery of the disease). This comparison shows that, although both devices helped COPD patients breathe better, the resistive RMT device provided greater benefits to COPD patients. [2]


The 2017 study
After 10 years, a study published in “Respiratory Medicine, again compared the effect of resistive RMT devices and threshold RMT devices in 60 stable COPD patients performing two 15-minute training sessions daily for 8 weeks. The patients were divided into three groups:
-
The first group used resistive RMT device
-
The second group used threshold RMT device
-
The third group didn’t perform RMT
Both of the groups using resistive RMT device and threshold RMT device showed significant improvements in breathing muscle strength, breathlessness, maximal exercise capacity, and quality of life as compared to the control group.
However, the improvement in quality of life was significantly greater in the group using resistive RMT device (36%) compared to the threshold RMT device (17%). Similarly, the improvement in exercise capacity was also significantly higher in resistive RMT group (22%) as compared to threshold RMT group (1.1%).
Again, this study demonstrates that resistive RMT device outperformed the threshold RMT device in benefiting the COPD patients. [3]
The 2024 study
Another recent study from “Respiratory Medicine” again compared the effect of a resistive RMT device and a threshold RMT device on 75 COPD patients performing two 15-minute training sessions daily for 8 weeks. The patients were divided into three groups:
-
The first group used resistive RMT device
-
The second group used threshold RMT device
-
The third group didn’t perform RMT
Both of the groups using the resistive RMT device and the threshold RMT device showed significant improvements in exercise capacity, breathing muscle strength, and breathlessness as compared to before training and from the control group at the end of the study.
Moreover, the group using resistive RMT device significantly improved the breathlessness, promoted deep and slower breathing along with an increased ventilation efficiency as compared to the group that used threshold RMT device. This study further strengthens the superiority of resistive RMT devices over threshold RMT devices. [4]
Where can I find the best resistive RMT device?
Now that scientific research has tilted the balance toward resistive RMT devices, your next important step is selecting the right RMT device that best suits your goals. High-quality RMT devices are available through official brand websites, trusted medical suppliers, and reputable online marketplaces like Amazon. However, it is critical to choose a clinically tested and FDA-registered device to ensure safety, effectiveness, and durability.


Devices like THE BREATHER have become favorites among respiratory therapists, physicians, and fitness experts due to their ease of use, versatility, and proven record of clinical benefits. With a legacy spanning over 45 years, THE BREATHER has empowered more than 2 million people to breathe better, recover, and enhance their performance, and continues to reach more patients every day.
How does THE BREATHER stand out among other RMT devices?
While most other devices focus only on inhalation or use a fixed threshold, THE BREATHER stands out because it offers resistive respiratory training for inhalation and exhalation in a single unit. It comes with adjustable resistance settings that allow gradual and personalized progression. Its lightweight design, simple dial adjustments, and versatility make it the optimal choice for patients, athletes, respiratory therapists, and fitness experts.
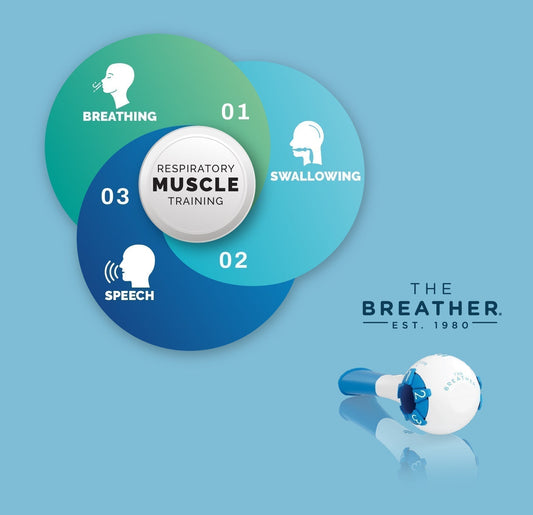
Moreover, in a range of clinical studies, THE BREATHER has been demonstrated to improve breathing muscle strength, endurance, speech, and swallowing function, stress, blood pressure, and quality of life.
How to use THE BREATHER?
Using THE BREATHER is straightforward. Here's how to get started:
Get ready
Sit upright in a comfortable position.
Adjust Resistance Levels
Understand your levels
THE BREATHER allows you to set inspiratory (inhale) and expiratory (exhale) resistance levels independently using the dials. This means they do not have to be the same, allowing for personalized training.
Setting your starting point
If you are working with a healthcare professional (such as a respiratory therapist, nurse, or speech-language pathologist), adjust both the inspiratory and expiratory dials exactly as they have recommended for your initial training.
If you are determining your levels independently, begin by turning the dials to the lowest resistance setting. Gradually increase the resistance until you find a level that feels challenging but still allows you to complete a full set of breaths comfortably, without feeling excessively strained, breathless, or lightheaded. A common initial sensation is similar to taking a deep, forceful breath through a straw. Always refer to THE BREATHER's user manual or accompanying instructions for detailed guidance on finding your optimal starting levels, how to progress, and important safety information.
Position Mouthpiece
Secure the mouthpiece firmly in your mouth, sealing it tightly with your lips to prevent any air leakage.
Breathe Deeply
Inhale deeply and forcefully through the device for 2 to 3 seconds. Immediately after, exhale with the same depth and force. Throughout this process, focus on generating the breathing force from your diaphragm (your belly), not from your cheeks.
A typical session consists of two sets of 10 breaths, twice daily, but this can be customized based on your goals and healthcare provider recommendations. Cleaning your breather device after using it is recommended. Wash the device regularly with mild soap and water, rinse thoroughly, and air dry.
Conclusion
Both resistive RMT devices and threshold RMT devices have proven their effectiveness. However, scientific evidence strongly supports the superior performance of resistive RMT devices, particularly regarding overall clinical outcomes, including better quality of life, reduced breathlessness, and improved exercise capacity.
With research pointing toward their effectiveness, the next step is selecting the right resistive RMT device that fits your needs. Devices like THE BREATHER offer a comprehensive solution, targeting both inspiratory and expiratory muscles, with adjustable resistance for personalized progress.